Sexual Health Information For Gay/Bisexual Men And Gender Diverse People
Syphilis has been on the rise among gay, bisexual, and other men who have sex with men (GBMSM) in Rhode Island. It can spread through oral sex or anal sex. Infectious syphilis was diagnosed in Rhode Island’s GBMSM population at a rate more than 165 times higher than in the heterosexual male population in 2020. A substantial percentage of GBMSM diagnosed with infectious syphilis in recent years are also living with HIV. HIV-positive men who are co-infected with infectious syphilis are more likely to spread HIV to their sexual partners than HIV-positive men who do not have infectious syphilis.
If left undetected and untreated, syphilis can lead to muscle movement difficulties, paralysis, numbness, gradual blindness, and dementia. You may have syphilis and not have any symptoms, so being tested for it by a doctor is important. It is also important to get tested for HIV and other sexually transmitted infections (STIs) such as gonorrhea and chlamydia.
The relatively high incidence of STIs among GBMSM may be related to multiple factors, including individual behaviors and sexual network characteristics. The number of lifetime or recent sex partners, rate of partner exchange, and frequency of condomless sex each influence someone’s probability of exposure to STIs. Rhode Islanders can order free condoms by mail from RIDOH at https://health.ri.gov/findcondoms.
Mpox (Monkeypox)
Sexually active Rhode Islanders should also be aware of the risk of mpox (also known as monkeypox), a rare, but potentially serious, viral illness which belongs to the orthopoxvirus family. While many of the identified cases of mpox are within networks of self-identified gay and bisexual men, gender diverse individuals and other MSM, people of any sexual orientation or gender identity can become infected and spread mpox.
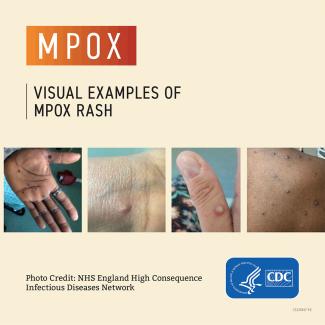
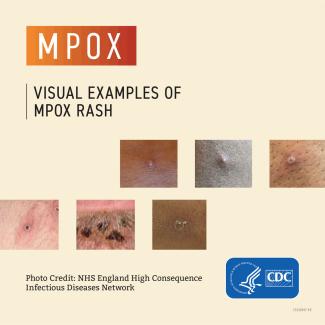
People with mpox typically have symptoms including a rash that can look like pimples or blisters that appears on the face, inside the mouth, and on other parts of the body, like the hands, feet, chest, genitals, or anus. Therefore, it is important to talk to your healthcare provider if you have an unexplained rash for evaluation.
Sometimes with mpox, people get a rash first, followed by other symptoms. Others only experience a rash. The rash goes through different stages before healing completely. Most infections last two to four weeks and resolve on their own, but some cases can become severe.
Public awareness is important as the disease could spread within potentially larger groups or networks of people. RIDOH urges the media, government officials and the community at-large to avoid stigmatizing a particular group or person for mpox, but rather support those at highest risk and ensure that all communities remain vigilant.
Key points to know about mpox:
- Be aware of mpox and how it is transmitted;
- Recognize the signs and symptoms;
- Be careful if you are having multiple sexual partners;
- Get tested if you have any signs or symptoms.
- For information about mpox vaccination, visit the RIDOH mpox webpage.
Vaccination
The JYNNEOS mpox vaccine is now available on the commercial market. CVS and Walgreens now have the mpox vaccine in stock and vaccine scheduling is available on the CVS and Walgreens websites or speak to the pharmacy for other scheduling options. Speak to your health insurer and/or pharmacy to determine if there is any out-of-pocket cost. If you do not have insurance, one of the following clinics may be able to assist you with vaccination options available through the State Supplied Vaccine program:
- Open Door Health (Providence) – 401-648-4700
- Corliss Clinic at The Miriam Hospital (Providence) – 401-793-2928 (At this location, vaccinations are available to eligible patients as part of a wellness appointment in the clinic. When calling, ask to schedule an appointment in the clinic. If you are specifically interested in the mpox vaccine, please indicate that so the provider will be aware. You still need to be evaluated by a provider. You will also be offered STI testing. The clinic has financial assistance services for patients who are uninsured or who have insurance with copays.)
If you have already been exposed, getting vaccinated as soon as possible after exposure to someone with monkeypox (ideally within 4 days) may help prevent the disease, or make it less severe.
Eligibility
Anyone of any sexual orientation or gender identity who is at risk for mpox can get vaccinated. Please see the mpox web page for detailed information about mpox vaccine eligibility and recommendations.
What you should do to prevent STIs
- All sexually-active people should get tested yearly, and perhaps more often if you have multiple sex partners. If your partner has an STI, you should get evaluated immediately.
- Tell your doctor or other provider that you would like to be tested. Your doctor will ask you some questions and will probably order some lab tests.
- If you have some STIs like syphilis, your doctor can treat you so that you are cured.
- After treatment, continue regular testing as your doctor recommends. You can be reinfected by many STIs, including syphilis.
- Always use a condom during anal sex.
- Avoid having oral sex with a man that has a sore/rash on his penis.
- Avoid having oral sex if you have a sore in your mouth. Learn more about Syphilis.
What you can do
- Learn about testing, treatment, and ways to protect yourself and your partners from HIV and sexually transmitted infections by checking out Your Health, Your Choice: Know Your Options, RIDOH’s Guide to Safer Sex.